Insider Interview
What are biomolecular condensates, and will they be a breakthrough in diabetes treatment?

Ameet Nathwani at Dewpoint Therapeutics considers the current treatment landscape for both type 1 and type 2 diabetes, as well as evaluating the use of biomolecular condensates as a potential treatment option
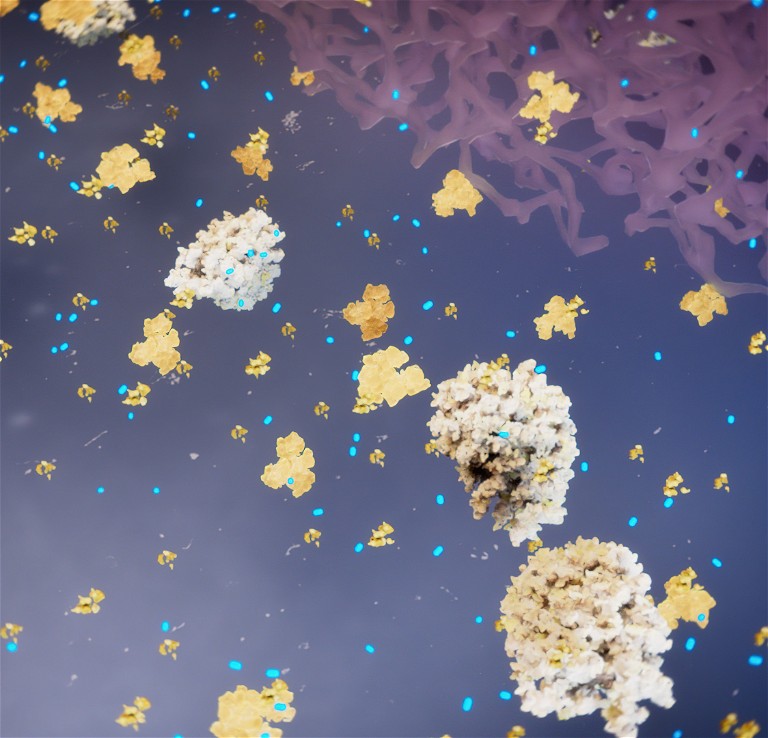
Condensate modifying drugs (c-mods here in blue) are uniquely designed to hit condensate targets and restore healthy condensate properties and function
Pharmafocus: What are the current standard-of-care treatments for type 1 and type 2 diabetes?
Ameet Nathwani (AN): Type 1 diabetes, also known as juvenile diabetes or insulin dependent diabetes, is a chronic condition with its onset usually occurring in childhood, when the pancreas produces insufficient insulin due to an autoimmune destruction of the insulin-producing cells in the pancreas. Insulin is a vital hormone needed to allow sugar (glucose) to enter cells in the body to produce energy. Patients with type 1 diabetes require insulin replacement as their mainstay of treatment; this can be administered through injections or pumps and needs to be accompanied by frequent or continuous blood sugar monitoring.
Type 2 diabetes, by far the more common form of diabetes comprising 95% of all diagnoses, is also a chronic condition. Unlike Type 1 diabetes, it results from the body’s inability to use the insulin effectively – acondition called insulin resistance – thereby leading to a relative insulin insufficiency. This is a progressive disease whereby the underlying insulin resistance not only leads to a progressive increase in blood sugar over time, but the insulin resistance itself contributes to additional complications including cardiovascular disease. One of the underlying risk factors for an increase in insulin resistance and type 2 diabetes is obesity, and in particular, central obesity – which is an excess accumulation of fat around key organs like the liver.
The mainstay of treatment in type 2 diabetes is a combination of intense lifestyle changes, regular blood sugar monitoring plus medication. The main first-line treatments include oral therapies such as metformin, but as the disease is relentlessly progressive, patients usually require multiple oral therapies over time including the addition of DPP-4 inhibitors, PPAR-gamma agonists and, in more recent years, the addition of SGLT2-inhibitors. However, these therapies are not considered disease modifying, and patients who continue to be poorly controlled, or who progress, will often transition to requiring insulin therapy or the addition of the newer class of injectable drugs such as GLP-1 agonists, which have shown promise in not only controlling blood sugar, but also in reducing weight and cardiovascular complications.
Apart from weight loss surgery (bariatric surgery), which is reserved for the most severe patients, no treatment has shown the ability to truly reverse or prevent the progression of type 2 diabetes, which explains the high unmet need. Given the epidemic proportions of the disease (nearly 550 million patients worldwide) and nearly seven million deaths every year (one death every five seconds), the global unmet need to be able to prevent or modify the course of disease is very high.
Pharmafocus: What are biomolecular condensates and how could they improve current diabetes treatments?
AN: A biomolecular condensate is a membrane-less compartment within a cell that forms when thousands of specific biomolecules, such as proteins and nucleic acids, come together in very specific ways to carry out specific functions when the cell requires them. Condensates are often formed through a process called liquid-liquid phase separation – akin to the separation of oil and vinegar in vinaigrette – where certain molecules become more concentrated in a particular region of the cell, they compartmentalise and self-organise to carry out a myriad of cellular processes, such as gene expression, signal transduction and stress responses. Condensates are thought to be important for the majority of biological functions in the cell.
The discovery of biomolecular condensates has completely transformed our understanding of normal cellular function and organisation. But the most important realisation was that if these membrane-less compartments form to regulate normal function, dysregulation of certain biomolecular condensates could be the root cause of many diseases and could pave the way to developing novel therapies that target the aberrant condensate. For decades, scientists have been trying to discover the underlying cellular triggers that lead to the development of type 2 diabetes. We know that one of the major biological precursors to the onset of this form of diabetes is the development of insulin resistance, where the tissues in the body become more resistant to the effects of insulin, and the body, therefore, has to produce more insulin to have the same effect. Over time, this demand of higher insulin levels cannot be met and that’s when the individual can transition to becoming diabetic. Research from MIT and Novo Nordisk found that the insulin resistance in tissues from patients with diabetes was caused by dysregulation of a condensate responsible for the efficient signaling of insulin in cells.
Industry collaboration in this area is focused on building upon these findings to discover what are the condensate dysregulations that drive the insulin resistance process, which then leads to diabetes. By doing so, we may finally be able to address a fundamental biological driver of type 2 diabetes and its progression. We are hopeful of being able to find small molecules or novel therapeutics that can modulate or normalise the insulin signaling process. If effective, these drugs could be added to any of the current therapies to improve glucose control and drastically slow down the progression of diabetes or, potentially, prevent the transition to full onset type 2 diabetes, if patients are diagnosed early enough in the prodromal or prediabetic stage.
Pharmafocus: How could AI be used to further expand the field of biomolecular condensates?
AN: Companies can use AI extensively in an integrated way in discovery processes, leveraging AI to develop digital condensate signatures. Teams can then visualise these subcellular compartments, tagging the key components of condensates inside the cells and extracting several thousand features from these images, which can then be compared with a library of compounds. These can correlate the very subtle changes of these images to the desired functional change of the cell’s response and can then quickly use this to find the chemical structures or even potential mechanisms that are causing favorable changes. From there, many companies will be using various AI tools to accelerate the optimal design of the molecules and their impact. Condensate images across multiple diseases and cell types and with thousands of compounds, help form the basis of a proprietary Knowledge Graph, which can be used to make predictions on linking genetics to condensates that are likely to be involved in diseases, and immediately predicting which types of compounds could be used to modulate the condensate, thereby accelerating the discovery process. The potential value of this Knowledge Graph to both academia and industry could be very significant, given the increasing realisation of the widespread involvement of condensates as central nodes of dysregulation in disease.
Pharmafocus: What are the possible obstacles to implementing biomolecular condensates as part of diabetes treatments?
AN: The only specific obstacle to being able to implement a condensate-targeted drug for the management of diabetes will be having the physicians fully understand and appreciate the new biology and its implications, as this field is very new. However, as the drug development process is lengthy and we would need to generate the compelling clinical data through conventional trials showing the disease-modifying potential, there is plenty of time to both educate and demonstrate the utility of this approach.
Pharmafocus: How do you see the diabetes treatment landscape developing in the next five years?
AN: It’s a very exciting time in the diabetes field. The recent approvals of the GLP-1 agonist therapies in both diabetes and obesity have opened up the field of addressing the impact of obesity in cardio-metabolic disease. There are many trials looking at the longer-term impact of managing obesity on both cardiovascular disease and the development of diabetes, which could significantly change the landscape in the future.
The recent advent of the SGLT2 inhibitors with very promising effects on both cardiovascular and renal protection have also been a very welcome advance and are leading to interesting new scientific avenues to explore regarding the underlying mechanism of these benefits.
Given the global magnitude of the diabetes problem, there is still a lot to do to really make an impact on the costs, complications and mortality of the disease.
Author Bio:
Since 2020, Ameet Nathwani has been chief executive officer of Dewpoint Therapeutics. Nathwani has more than 25 years of experience in the pharmaceutical industry. Before joining Dewpoint, he was an executive committee member at Sanofi SA, where he also served as chief medical officer and chief digital officer and was responsible for enhancing Sanofi’s strategy to integrate digital technologies and medical science to ultimately improve patient outcomes across the portfolio. Prior to that, Nathwani worked for over 11 years at Novartis Pharma AG, where he served as global head of medical affairs and as member of the pharma executive committee and held different senior development and commercial positions. Nathwani also worked in senior roles in R&D at GlaxoSmithKline, SmithKline Beecham and Glaxo Group Research in both the UK and US. He earned his medical degree from the University of London, specialised in cardiology and intensive care medicine, and holds a Master of Business Administration.